The Don Margolis Blog
Featuring the most comprehensive collection of "disease specific" stem cell treatment articles in the world. We provide the most current, factual and comprehensive information on available stem cell treatments today for your specific medical condition.
NEED STEM CELL INFO RELEVANT TO YOU?
Go to the
MEDICAL CONDITION column to the left to search our extensive database of stem cell treatment articles.
----------
I'M READY FOR TREATMENT!
-
Go to TREATMENT INFORMATION and fill out the medical form to receive personalized information on stem cell treatments for your specific condition.
-
Watch the video below for immediate information.
I WANT THE LATEST STEM CELL TREATMENT INFORMATION!
-
Go to NEWSLETTER SIGN UP to receive regular updates on stem cell treatments for multiple diseases.
WHO IS DON MARGOLIS?
----------
Still can't find what you're looking for?
For more specific searches, use the search bar at the top right or contact a patient coordinator at:
214-556-6377
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
A 71 year old male suffering from congestive heart failure had a left ventricular assist device (LVAD) put in his chest, but his recovery may also have to do with the fact that his treatment included injections of his own bone marrow stem cells. The patient is taking part in a cutting-edge study at the University of Minnesota, where researchers hope that stem cell therapy could eliminate the need for transplants.
Stem Cell Therapy Offers Hope of Eliminating Need for Heart Transplants
Allan Isaacs, 71, had congestive heart failure, which made it difficult to perform basic tasks such as walking, breathing and eating.
But after getting a left ventricular assist device put in his chest, he got moving again.
The LVAD helps pump oxygen-rich blood throughout the body, but Isaccs' recovery may also have to do with the fact that his treatment included injections of his own bone marrow stem cells. Isaacs is taking part in a cutting-edge study at the University of Minnesota.
"We isolate the stem cells and when they go in for surgery we inject those cells on the heart wall," said Dr. Ganesh Raveendran,
director of the Cardiac Catheterization Laboratory at the University of Minnesota Medical Center.
One-third of the patients receive a placebo, and the rest get 10 injections of stem cells into their hearts.
Muscle tissue is then analyzed to see whether the cells have transformed into cardiac muscle or made other meaningful changes.
In many cases, an LVAD is a bridge to a transplant, but the hope is that the stem cell therapy could eliminate the need for a transplant.
The research team at the University of Minnesota Medical Center hopes to wrap up the study by the end of the year before launching a much bigger national study.via
Am I a Candidate for Heart Stem Cells?
Posted:
11/9/2013 12:00:00 AM by
CJ Simpson | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
Poets say your Eyes are the Windows to your Soul; now Science has just caught up:
YOUR EYES ARE THE WINDOWS TO YOUR HEART!
Research on the eyes as windows to potential cardiovascular disease risk and dysfunctional coronary artery flow in prediabetics.
Eyes Provide Early Clues to CV Risk
Greek researchers presented three studies showing how retinal circulation could potentially distinguish patients who are at a low short-term, but high lifetime risk, of cardiovascular (CV) adverse events from those who are at a low short-term and low lifetime risk.
One study, involving 229 stage I-II never treated essential hypertensive patients with a median age of 62, found a significant correlation between deterioration of the retinal vascular category (stages 0 to 4) and impaired ejection fraction. There also was an increase in interventricular septum end-diastolic thickness and left atrial anteroposterior diameter.
A second study, which looked at 268 consecutive newly diagnosed, untreated, essential hypertensives with no history of diabetes or CV disease and a median age of 60, found a parallel escalation between retinal vascular alterations and arterial stiffness, measured by pulse pressure.
The third study, examining 202 consecutive patients with newly diagnosed hypertension without CV disease and a median age of 60, found a significant correlation with the stage of retinal vascular damage and metabolic syndrome.
Lead author of all three studies Vasiliki Katsi, MD, from Hippokration General Hospital in Athens, said in a statement that fundoscopy, the method of measuring retinal vasculature, is currently too subjective and would benefit from automated software.
Compression Rare with This Stent
A review of 2,936 Promus Element stents implanted during a 22-month period found a 1.44% per patient longitudinal stent compression rate, Michael Gick, MD, from the Heart Centre Bad Krozingen in Germany, and colleagues reported.
The mean age of patients was 67 and the rate of stent compression per lesion was 0.70% and per all stents was 0.68%.
The only significant predictors of stent compression were stents placed in the ostial segments (OR 8.33, 95% CI 3.30 to 21.28), number of stents implanted (OR 1.57, 95% CI 1.01 to 2.45), and the presence of a bifurcation(OR 3.57, 95% CI 1.36 to 9.35).
They concluded that longitudinal stent compression with the third-generation Element stent is rare.
Consensus Paper Focuses on CRT in HF.
The increased use of cardiac resynchronization therapy (CRT) in heart failure -- more than 200,000 devices implanted worldwide last year -- has led to an expert consensus statement on the practical management of these patients.
"Our goal was to establish a consensus statement on how to manage CRT patients before, during, and after the implantation procedure," said lead author Jean-Claude Daubert, MD, of the University of Rennes, France, in a statement. Daubert said that solid clinical evidence was lacking for all aspects of managment.
The document, developed by an international team from North America and Europe and released at the ESC meeting, is divided into six sections:
- Pre-implant evaluation
- CRT implantation
- Predischarge evaluation and device programming
- CRT follow-up
- Response to CRT management of the nonresponder
- Special considerations
In the pre-implant evaluation section, for example, the focus is on potential temporary contraindications to the intervention, and how to manage medications, particularly anticoagulants and antibiotics, just before and during the implantation procedure. Daubert said there was no consensus before on these particular aspects.
The statement has been published in EP Europace and HeartRhythm (2012;9:1524–1576), and can be downloaded at the European Heart Rhythm Association website.
Guidelines Come from Industry-Sponsored Studies
Industry-sponsored studies make up the bulk of class I recommendations in the 2011 ESC Guidelines for Acute Coronary Syndrome (ACS) without ST Elevation, researchers found.
This same group of researchers, led by Payal Kohli, MD, of the University of California in San Francisco, had previously found similar results for the guidelines pertaining to the management of patients with unstable angina/non-STEMI developed by the American Heart Association/American College of Cardiology.
For the current study, of the 85 citations used to support class I recommendations, they found 84% of them were funded by non-government or industry sources.
They noted that recommendations for pharmacological therapy had a higher percentage of industry support than other areas including secondary prevention, special populations, and diagnosis and intervention.
They concluded that industry-sponsored studies have a positive impact on clinical guidelines "in identifying many new strategies and treatments for ACS."
Diabetics Have Slow Coronary Blood Flow
Coronary blood flow is slow in prediabetic and diabetic patients with normal coronary arteries when compared to nondiabetics, a retrospective study found.
Researchers reviewed the angiograms of 759 patients with normal coronary arteries (left anterior descending artery, left circumflex, and right coronary artery) for TIMI frame counting.
They found significant differences in frame counts between nondiabetics, prediabetics, and diabetics in each artery, reported Ugur Arslan, MD, from Samsun Education and Research Hospital in Turkey, and colleagues.
In a second post hoc analysis, they found that prediabetics and diabetics had similar TIMI frame counts for all three coronary arteries, but both of these groups had significantly higher TIMI frame counts than nondiabetics.
"We have revealed for the first time that patients with prediabetes have slow coronary flow measured by TIMI frame count just like diabetic patients when compared to nondiabetics," they concluded.
They suggested that this abnormality "may show the endothelial dysfunction in the coronary arteries which develops in the prediabetic phase before overt diabetes mellitus arises."
From the American Heart Association:
Science News: ESC Congress 2012
Posted:
9/5/2012 8:14:57 PM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
According to a pro-life research organization, the lackluster success rates have made funding for embryonic stem-cell research more difficult to come by.
A new report from the education and research arm of the Susan B. Anthony List shows that the scientific community now recognizes that "morally unproblematic alternatives to embryonic stem cells [are] the best hope for progress toward effective treatments and therapies."
The scientific community now understands that the best chance for success with treating medical conditions is through adult stem cells.
"We've analyzed the last five years of funding by the San Francisco-based California Institute for Regenerative Medicine (CIRM), which was created to promote embryonic stem-cell research that hopefully would lead to therapies and cures for various diseases," Donovan explains. "It was promised to do that. Our analysis shows that they have been unable to find projects that work that way, and they are now turning more and more to adult stem-cell resources, which do not raise those ethical issues of destroying human embryos."
While no successful uses of human embryo research have been found, research with adult stem cells has shown promise in treating over 70 diseases and medical conditions.
Donovan concludes the survey shows that even the most supportive entity in the country, CIRM, cannot find beneficial projects for human embryo research and is turning to adult stem cells.
Posted:
8/29/2012 8:27:46 PM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
By SHANNA SISSOM | Herald Managing Editor
At age 53, Kent Winders hopes to pick up his grandchildren for the first time and ride a horse again.
“I have nine grandchildren and I’ve never picked one up,” Winders said. “It’s been a goal in my life ever since my (grand) babies were born.”
The disabled former New Mexico rancher has lived in Plainview’s Prairie House Living Center for three years, making friends throughout the assisted living center while being near his son and daughter-in-law, Cory and Jennifer Winders.
Winders suffers from a rare form of multiple sclerosis, known as primary progressive, is wheelchair-bound and also has very limited use of his upper extremities.
The bulk of his mornings are spent in therapy and in the afternoons — at least when a Texas Rangers game isn’t on — he often roams about in his motorized wheelchair. He knows where every item in Walmart is located, and he often fetches merchandise his fellow residents want to buy. Sometimes he goes over to Chili’s or Tractor Supply.
He taught a Bible study at the nursing home for over a year, but just reading Scriptures is challenging anymore.
“I can’t even hold my Bible now,” he explained.
But he likes to look at pictures of his grandchildren, and is happy to show them off to a visitor.
Despite his predicament, Winders is hopeful a procedure relatively new in the United States could help him. And he has reason to believe it will.
Back in 2001, he received a stem cell treatment in Tijuana, Mexico, and saw noticeable improvement to his overall condition, among them were regaining bladder control and seeing his swollen purple feet return to normal size. Friends helped him with costs associated with it all, and the volume of stem cells he received were 3 million to 5 million.
By vast contrast, stem cell infusions now available in the Houston area could deliver up to 600 million stem cells in multiple injections of 100 million to 150 million each, he said.
Winders has been researching all this with his daughter, who’s made contact with Hale County native physician Stanley Jones who performs these procedures in the Houston area. He’s even talked to Texas State Rep. Rick Hardcastle, who himself has undergone stem cell infusion for MS.
“It’s been the most miraculous thing that’s ever happened in my life,” Hardcastle told the Herald. Before he had the infusion, being out in the heat for long would leave him crippled, and he had enormous problems balancing. “Basically I got better.”
Four days after his infusion almost a year ago, Hardcastle said he was on a long-planned trip to Alaska, standing in a river fishing,
“I started getting better, and anybody that asks me, I say call me any place, anytime,” Hardcastle said.
And so he has encouraged Winders to get the stem cell procedure. Winders is quick to point out the stem cells would all be harvested from his own stomach.
“Those stem cells are not controversial. They are not embryo, not harvested from aborted babies,” Winders said. “People who have the same faith as I do would want to know that.”
He’s been fighting MS for about 24 years, but his particular type of MS affects only 10 percent of those suffering from the illness, and there’s no prescription drugs available to that group.
When he talked to Hardcastle recently the state representative encouraged him to seek the treatment, but the $28,000 price tag and travel expense is cost-prohibitive.
However, his friend Danny Andrews is among those who hope that just maybe donors might come forward to help the man Andrews calls his hero.
“He’s been such an inspiration to me because of his faith and desire to get out of that chair,” Andrews said. “He’s still a young man and I think he feels somewhat trapped there, and I hurt for him so badly.”
Andrews, who carries on an informal personal ministry at the facility, came across Winders during one of his weekly visits not long after Winders arrived at the facility. The two made an instant connection, Andrews said. In addition to their strong religious faith, they both are avid Texas Rangers fans.
“Me and Danny coach the Rangers from Plainview,” Winders joked from his room recently.
So as family and friends try to figure out how to raise money for the stem cell infusion Winders believes will change his life and enable him to pick up his grandbabies, he remains faithfully optimistic.
“I’m 53 in a nursing home and I don’t want to live here all my life,” Winders said. “I’d like to regain my independence, support myself where I can live on my own and do normal everyday activities everyone else does.”
The Winders family currently is researching ways to raise money, and hopes to establish a fund soon.
“Lord, I hope someone would come forward to help,” Andrews said about his friend.
Posted:
8/19/2012 2:54:30 PM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
Time to heal: Brian Hogan relaxes by listening to music after receiving treatment in a centre in Beijing last week
By Anne Sheridan
Published on Monday 13 August 2012 14:00
FOR BRIAN Hogan and his family there are only three things left for them to do - wait, hope and pray.
The 35 year-old has now returned home to Limerick after three weeks in China, where he underwent stem cell infusions in the hope that one day he might be able to see and walk again.
However, it could be a long and anxious wait as the Ballykeeffe family have been told by doctors in Beijing that it could take six to eight months for the controversial treatment to work.
“We’ve had a good time in China and they’ve treated us well. The treatment is over so we just have to play the waiting game now to see what improvements I receive..it’s going to be an interesting wait,” said Brian, in an online video message, where he thanked people for their support.
Over the course of three weeks, Brian received stem cell infusions every second day, as well as lumbar punctures, and a number of therapies and exercises to improve his mobility.
He was based in a Beike Biotech treatment centre in Beijing, which uses stem cell products derived from umbilical cord, cord blood, and bone marrow stem cells. While the treatment continues to attract controversy and no funding was available from the Irish State as these are experimental trials, his family said anyone in their position would love to see him being able to reclaim the life he lost three years ago.
On July 19, 2009, Brian suffered severe brain damage and was left blind and partially paralysed after an unprovoked attack in Nottingham in the UK, where he was working as a senior quantity surveyor for a construction company.
His sister Nevis said while the treatment is “very exciting”, they are also “sick with nerves” in case they don’t see the results they’re hoping for. “Brian is so positive and always tries to keep the bright side out. He still enjoys life. He never has a woe is me attitude,” she added.
After he spoke out about his condition last September through the Limerick Leader newspaper, two wealthy female donors stepped forward and donated a total of €10,000 to help with the costs of his medical treatment, after being moved by his story. Nevis said they are grateful for “every penny” people have donated, as the treatment and other costs amounted to €40,000. In the past week, donations have continued to come in from people in Armagh, Derbyshire and Colorado.
Posted:
8/14/2012 1:56:11 AM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
Heart bypass surgery and other complicated procedures which require healthy blood vessels may soon be using vessels grown from adipose, or 'fat derived,' stem cells. Through liposuction, doctors can collect hundreds of millions of stem cells that can be used to generate blood vessels. The cells being ‘autologous’, or from the same patient, have no risk of adverse reactions or rejection.
Can liposuction help you live longer?
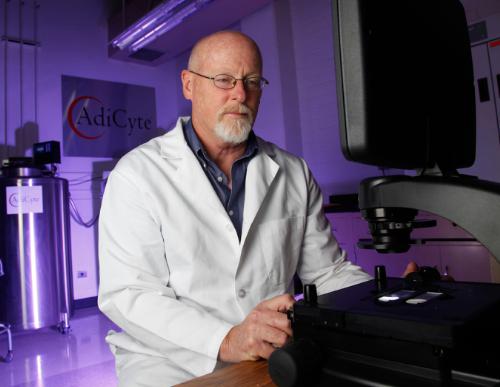
TUCSON, Ariz., Aug. 9, 2012 — Doctors at the University of Oklahoma reported the first successful procedure for growing new blood vessels from adipose, or ‘fat derived,’ stem cells. These newly formed blood vessels can be used in heart bypass surgery and other complicated procedures requiring healthy vessels, according to the researchers, who presented their findings at the American Heart Association’s 2012 Scientific Sessions. The ability for a patient and doctor to literally pre-order new blood vessels for a heart bypass patient is exactly what AdiCyte, an adipose stem cell cryogenic bank, is all about. Storing an individual’s adult adipose tissue and stem cells for their future use in regenerative medicine, tissue engineering and cosmetic or reconstructive procedures.
Through liposuction, doctors can collect hundreds of millions of stem cells that can be used to generate blood vessels. The cells were “seeded” onto a ‘bio-scaffold’ and as they multiplied, researchers rolled them into tubes with the diameter of small blood vessels. Within weeks, new, healthy tissue began to grow into usable blood vessels. And since the cells are ‘autologous’, or from the same patient, there is no risk of adverse reactions or rejection.
But one of the key considerations is the age of the patient and thus the age of the stem cells. Young stem cells are much more active and potent than older cells. And young blood vessels are much more functional than older vessels.
One potential downside is that these blood vessels take time to grow in the lab. “They would not be available immediately, but you could bank your own cells and keep them until the time comes that you need them,” said Dr. Roberto Bolli, an American Heart Association spokesman and chief of cardiology at the University of Louisville in Kentucky.
Success using stem cells in tissue engineering have led to just that-the option for patients to bank their adipose stem cells as a biological resource for use in the future in tissue engineering and regenerative medicine.
Dr. David Harris, Professor of Immunology at the University of Arizona in Tucson, is Chief Scientific Officer and founder of Adicyte(TM), an adipose stem cell cryogenic bank. AdiCyte uses modern cryopreservation methods to safely store an individual’s adult adipose tissue and stem cells for their future use in regenerative medicine, tissue engineering and cosmetic or reconstructive procedures.
“Adipose tissue is the richest source of mesenchymal stem cells (MSCs) in the human body, and more than 100 FDA clinical trials are in motion to help bring these cellular therapies to approved indications” said Harris.
For $985, patients can save their adipose tissue and stem cells, and request them whenever needed. There is an annual maintenance fee of $120. Cryogenic storage of the tissue in essence, ‘stops the clock’ on cell aging, so if the cells are needed twenty years from now, they will still have the same level of vitality and activity as when they were banked.
“The ability for a patient and doctor to literally pre-order new blood vessels for a heart bypass patient is exactly what AdiCyte is about,” says Scott Edelman, AdiCyte’s CEO and co-founder. “We want to help drive the advancement of regenerative medicine by enabling people to preserve their youngest stem cells possible, so they have the opportunity to take advantage of these miraculous new technologies and live longer.”via
Posted:
8/10/2012 12:00:00 AM by
CJ Simpson | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
A group of local doctors on Wednesday injected grown stem cells into a severely-burnt Malaysian woman to repair her skin.
In an extremely rare procedure, doctors extracted, cultivated and then injected adult stem cells into the woman to treat intractable burn scars, experts said.
Doctors with JK Plastic Surgery Center in Seoul said the surgery on 19-year-old Hui-Linn was successful. The women’s body was scarred after her father Lim Teik Swee splashed acid on her mother and her while they were sleeping at home on Oct. 24, 2009. The mother died of her injuries.
Hui-Linn lost the sight in her right eye and had nearly all of the skin on her face severely burnt. Her other eye has limited vision.
The doctors said stem cell injections were the best way to allow Hui-Linn to smile and make other facial expressions.
“We have already performed surgeries on Hui-Linn to recover her eyebrows, and the lower lip and jaw areas last year. However, we needed something beyond plastic surgery because the scarred area was vast and she needed more flexibility and elasticity to the skin while her wounds are too deep to be covered by other methods such as skin transplantation. Stem cells could transform and grow into her skin, giving her comfort and convenience in moving her facial skin,” said Dr. Joo Kwon, chief of the JK center.
Dr. Bae Jun-sung, who will be overseeing her treatment, said Hui-Linn will be injected with a total of 90 million adult stem cells contained in 18cc of liquid over four sessions.
The stem cells were extracted from her bone marrow in June and were cultivated by PharmiCell, the only company here authorized to cultivate and commercialize stem cells.
Hui-Linn, who wore makeup and a bright-colored outfit to the press release held at the hospital, said she is thrilled to receive the treatment.
“For the past several months I have made Korean friends and am learning Korean, too. I cannot wait to start the treatment and a new life!” she said.
By Bae Ji-sook (baejisook@heraldm.com)
Posted:
8/2/2012 5:23:05 AM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
In a Tissue-Engineering First, Doctors Think the Boy's New Windpipe Could Grow
By Brenda Goodman, MA
WebMD Health News
July 25, 2012 -- Ciaran Finn-Lynch is an accidental medical pioneer. With his life in danger, doctors used the 13-year-old's own stem cells to grow him a new windpipe, and they did it inside his body -- a feat that's never been accomplished before.
"It's a really heroic story," says Harald C. Ott, MD, an instructor of medicine at Harvard Medical School in Boston. "They really saved this kid's life."
Ott worked out some of the science that made the procedure possible but was not directly involved in Ciaran's treatment.
Two years after the surgery, doctors say Ciaran (pronounced KEER-an) is living the life of a normal teen. He's grown more than 4 inches and gone back to school. Best of all, he has no need for an expensive and complicated regimen of anti-rejection drugs.
What doctors are learning from his case could help thousands of children born each year with life-threatening birth defects.
An Urgent Medical Need Drives a Discovery
Ciaran was born with a windpipe so small and deformed that it caused his lungs to collapse.
Doctors managed to hold his airway open using metal tubes. But eventually the tubes eroded into his aorta, the large vessel that carries blood out of the heart. He was rushed to the hospital with massive bleeding. Twice.
The second time, the bleeding stopped on its own. That gave his doctors a small window of time to look for other options.
Two years earlier, scientists had devised a new way to create organs using a patient's own stem cells. Though the technique had only been tried in adults, they thought the same method might work for Ciaran.
Working quickly, his doctors located a trachea, or windpipe, removed from a 30-year-old Italian woman whose organs were donated after she died. The trachea was about the same size and shape needed to replace the deformed one that Ciaran was born with.
Scientists in Italy cleaned the organ of all its cells using a method discovered at Harvard Medical School. Working with a detergent found in shampoo, they were able to strip the cells away from the protein scaffold they grew on. It's a bit like remodeling a house by first tearing it down to the studs.
That step was important because it cleared away any markers that might have caused Ciaran's immune system to reject the transplant.
Back at Great Ormond Street Hospital, a children's hospital in London, doctors removed stem cells from Ciaran's bone marrow. Stem cells are uniquely flexible cells that can be coaxed to grow into nearly any kind of tissue. The cells were sent to a specialized lab to be purified and returned to the hospital the same day.
After surgeons sewed the stripped-down donor windpipe in Ciaran's chest, they coated it with his purified stem cells. They also injected the tissue scaffold with proteins that encourage cell growth. For good measure, they took tissue samples from Ciaran's own trachea and placed those inside the tube of the windpipe with the stem cells. The tissue samples acted like blueprints, giving the stem cells instructions for what they should become.
The 'Holy Grail' of Tissue Engineering: Organs That Grow
Ciaran's case, which is reported in The Lancet, is the first time doctors have rebuilt an organ inside the body. Normally, donor organs are washed, reseeded with stem cells, and then grown in a lab until they are ready to be used in a patient. The process takes several weeks.
"We did not have the time to engineer and to culture the cells in a bioreactor because this child needed to have something done quickly. We used the child, himself, as a bioreactor," says researcher Paolo De Coppi, MD, PhD, one of the surgeons who treated Ciaran. "For him, there was no other option."
Worldwide, just 12 tissue-engineered tracheas have been transplanted into patients. Ciaran is the first child to get one. Doctors are watching him closely to see if the new trachea will keep up with his growth spurts. Since he's already shot up more than four inches since the operation, doctors think there's a good chance it will.
"We believe the matrix of the transplant will remodel with time. So it should allow, when the child grows, for the transplant to grow with the child," De Coppi says.
About 3% of babies are born with organs or tissues that are so malformed they threaten the child's life or growth. About 2% of newborns have poorly developed windpipes or lungs.
If tissue-engineered grafts like the one Ciaran has could grow, doctors think the damaged parts could be replaced almost as soon as they're discovered.
"A lot of kids, like kids with heart defects, any sort of structural defect that needs repair, if you do a repair with something that doesn't grow with the patient, you're committing them to a series of operations," Ott tells WebMD.
"So the holy grail of tissue engineering is to come up with something that is so integrated into the human body that it grows with the human body," he says. "That would make a big difference."
Posted:
7/26/2012 2:18:52 PM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
Michele Bachmann is the owner of Grapes 2 Glass Wine Boutique, 10351 Washington Ave., Suite 200, in Sturtevant. Bachmann has overcome a very aggressive form of cancer, thanks in large part to a stem cell transplant. She initially was given 18 months to live, or until she’d need another transplant. She’s had neither and is still in remission six years later. In the past, the average survival for her type of cancer has been two to three years.
RACINE COUNTY — After more than four decades, Michele Bachmann knew her body well enough to know there was something definitely wrong.
Yet it would be almost a year of frustration, aggravation and suffering before her feelings would receive validation — ultimately landing her in a grueling fight to save her life.
“I kept saying I was sick. People thought I was crazy,” she said. “I just kind of felt off, tired. Things just weren’t right.”
Bachmann, 50, who lives in Racine, said she contacted the doctor, who ran some blood tests.
“He said everything was fine. He said I just need to lose some weight and sit at my desk properly,” Bachmann said, giving her head a slight shake.
It wasn’t until later that she learned those tests results showed something more: Her white blood cell count was high.
“He said ‘oh no, you need to exercise, lose weight, take vitamins,’ ” she said. “By the time I got diagnosed in August, my spleen was the size of a basketball and weighed 25 pounds.”
It was about 11 months from the time she first knew she was sick before Bachmann — who owns Grapes 2 Glass Wine Boutique, at 10351 Washington Ave., Suite 200, in Sturtevant — received the proper diagnosis. It just wasn’t the one anyone wanted to hear.
She was in so much pain one day that she couldn’t make it to work in North Chicago, Ill., where she was a wine consultant. Her doctor was on vacation, so she went into prompt care. They took some blood, and she went home to make lunch, she said. They called her to come back because she was so low on blood. She received a transfusion, requiring three or four units, she said.
While at the hospital with her husband, parents and a friend, a doctor walked into her room, Bachmann recalled as if he stepped through that door only yesterday.
“He said ‘we just got the test results. You have leukemia,’ ” she recounted. “Everyone was in hysterics. It was a relief to me. I knew I was sick.”
He performed her first bone marrow biopsy while she still was in Wheaton Franciscan-All Saints hospital, 3801 Spring St., she said.
“It was probably one of the most horrible things I’ve ever done,” Bachmann said. “I was holding onto the railing of the bed and I probably could have broken the railing.”
But the doctor there wasn’t familiar with the type of cancer she had, Bachmann said.
Bachmann, who has nine siblings, said she called her sister, who had just completed a three-month course of chemotherapy at Froedtert Hospital in Wauwautosa because of tumors along her spinal column.
Her sister’s doctor recommended a new doctor at Froedtert, Timothy Fenske, Bachmann said. Fenske, a medical oncologist at Froedtert & The Medical College of Wisconsin, said he started working at the hospital in July 2005, and met Bachmann the following month.
He said she had mantle cell lymphoma. It is a type of non-Hodgkin’s lymphoma, he said.
“She had a lot of disease in her system,” Fenske said.
So she had a choice — the first of multiple tough decisions.
“They said where you’re at, you’ve got about two weeks to live. They explained my cancer is mainly in older men,” Bachmann said. “They said it’s only 4 percent of the types of leukemias and lymphomas. (Fenske) said ‘we could make you comfortable, or we could have you try this clinical going on right now.’ ”
But the course of treatment would be very strong.
“I said ‘if I’m gonna die in two weeks, what does it matter?’ ” Bachmann said.
She began her first chemo treatment in August 2005, and it truly was brutal, she explained. She developed sores inside her mouth. She lost her hair. She repeatedly lost her lunch. She became so weak she barely could move, she recalled.
Fenske said because Bachmann was so strong and young, and had such an extensive family support network, he suggested she undergo this type of high-dose chemotherapy. The average age of patients with Bachmann’s type of lymphoma is 63, he said.
“I thought chemo was chemo,” said Michele’s husband, Steve Bachmann. “Apparently there are hundreds of types.”
Looking back, Michele Bachmann can laugh at one type of chemo. She said the warning that came with it basically stated if she was allergic to eating rats, she might have a problem with it.
“I said, ‘well, I’ve never eaten rats, so we should be OK,’ ” she laughed.
“She’s one of our favorites,” Fenske said of Bachmann, in part because of her sense of humor. “Some people are a real challenge to get through chemotherapy. She was a trouper through it. Some people are really high maintenance.”
Often during chemo, patients’ sense of taste will be affected.
“Her thing was pickles,” Fenske said with a laugh. “She’d have this huge jar of pickles (when she came for chemo). I don’t know how many she’d work through.”
He said he suggested this type of aggressive chemotherapy because he wanted to send Bachmann’s cancer into remission, then dose her with stem cells he would transplant into her.
Stem cells are found throughout the body, including in bone marrow. Stem cells are a very basic building-block type of cells. In stem cell transplants, a batch of healthy cells is inserted into the body.
Froedtert spokeswoman Nalissa Wienke said “stem cell transplants are often the last best hope for patients.”
To help Bachmann’s body rebuild, Fenske gave her another choice, Bachmann said. She could use her own stem cells, or receive a transplant from a donor — such as one of her siblings. She chose her own stem cells, receiving the transplant Feb. 15, 2006.
Fenske said there are pros and cons to using one’s own stem cells and to using a donor’s.
Using one’s own stem cells allows doctors to administer high-dose chemotherapy, which works better at treating this type of cancer, but can leave patients without functioning bone marrows, Fenske said.
Transplanting the patient’s own stem cells also allows patients to recover better from this more aggressive, high-dose chemotherapy, Fenske explained. And it carries less of a risk — just 1 percent to 2 percent — of infection or a serious complication, he added.
So in Bachmann’s case, “it’s her own immune system coming back,” Fenske said.
But when a donor’s stem cells are used, patients would have to take anti-rejection drugs. And, they have more risk of infection, Fenske explained, at 15 percent to 20 percent.
“Historically, (with) the type of lymphoma she had, the average person only lived two to three years after diagnosis. In recent years, the prognosis has increased dramatically,” Fenske said.
Now, 50 to 60 percent of patients who receive high-dose chemotherapy and their own stem cells still are in remission six years later, Fenske said — just as Bachmann is.
An 8- to 10-year period is considered a good length of remission, Fenske said. And if it returns, he said Bachmann still could have a stem cell transplant from a donor.
“I’m just extremely, extremely happy” to be cancer-free for the past six years, she said. “I feel good.”
During the first couple of years after chemo and the transplant, she said she was waiting for the cancer to come back, almost preparing for it.
“(Now) if I feel run down, I know I didn’t go to bed early enough. I don’t have that really crappy feeling anymore,” Bachmann said. “Now I’ve got two birthdays. One in April and one on Feb. 15 — that’s my new life.”
Posted:
7/18/2012 4:37:01 AM by
Don Margolis | with
0 comments
Are you or a loved one interested in receiving stem cell treatment? For free information, please fill out our
treatment form or email me
don@repairstemcells.org and just put TREATMENT in the subject box and the MEDICAL CONDITION in the message.
 Madeleine Connor, 2, underwent an experimental procedure using her own cord blood stem cells to repair damaged tissue in her ear and restore her hearing. (Courtesy Stephanie Connor)
Madeleine Connor, 2, underwent an experimental procedure using her own cord blood stem cells to repair damaged tissue in her ear and restore her hearing. (Courtesy Stephanie Connor)
A
virus infection Stephanie Connor acquired during pregnancy put her unborn daughter at significant risk for brain damage and lifelong hearing loss.
"It was traumatic," said Connor, of LaBelle, Fl, after learning about her daughter's condition. "It was like mourning the loss of a child."
At age 1, baby Madeleine was completely deaf in her right ear and her hearing was severely lost in the left, said Connor. While a hearing aid helped to amplify some sounds for Madeleine, it would never fully repair the damage in her ear.
But a simple experimental procedure that Connor enrolled in for Madeleine may have restored her hearing and reversed her condition.
In January 2012, Madeleine, 2, became the first child to undergo an experimental hearing loss treatment through an
FDA-approved trial at Memorial Hermann-Texas Medical Center that infused stem cells from her own banked cord blood into her damaged inner ear.
Within the last six months, Connor says she's seen a dramatic improvement in Madeleine's ability to hear.
"Before, when she would hear something she would look all around," Connor said. "But now we notice that she turns in the right direction of the sound."
Madeleine was also able to speak for the first time, Connor said.
For more than two decades, umbilical cord blood transplantation -- either by a baby's own cord blood or another's, depending on the type of procedure -- has been used to treat otherwise fatal diseases including blood disorders, immune diseases, and some types of cancers.
Infusing cord blood stem cells into the body may also have the potential to heal and regenerate damaged cells and tissues.
Regenerative therapy using cord blood stem cells is currently being studied as therapies to treat conditions including cerebral palsy and brain injury.
For the first time, doctors are experimenting with cord blood stem cells to regenerate hearing in children who have suffered hearing loss.
This yearlong study will follow 10 children, including Madeleine, ages 6 weeks to 18 months, who have acquired hearing loss and who have banked their cord blood with the Cord Blood Registry.
"There are a number of treatments for hearing loss, but most of them rely on amplification of noises, not reversal of the hearing loss," said Dr. Samer Fakhri, associate professor and program director in the Department of Otorhinolaryngology at Memorial Hermann-Texas Medical Center, and principal investigator of the study.
Since Madeleine is part of a study that is currently under way, it's unclear whether Connor's perceived improvement of Madeleine is really due to the stem cell procedure.
Madeleine has already had one follow-up appointment to test her speech and language development, which are indicators that her hearing has improved. She will have another one mid-July.
Fakhri said it's still too early to determine whether the procedure benefitted Madeleine, or may be beneficial for other children.
"If there's any improvement, it should be detected within six months to a year," Fakhri said. "We can't determine from just one child if there's an overall benefit."
If the study results show significant improvement overall among the collective children studied, children with acquired -- not genetic -- hearing loss, may be able to benefit from the procedure.
"We do not recommend that stem cells at this point now should be a treatment modality for hearing loss," Fakhri said.
Previous studies in mice suggest long-term hearing repair after stem cell infusion. Fakhri says it's likely that if the procedure works, children like Madeleine will have long-term restored hearing.
"The way the stem cells work is they support repair," said Fakhri. "Once you repair the damage, there's no suggestion that it will dwindle over time."
Connor said the improvement she has seen so far is enough that she is grateful that she enrolled in the trial, and she hopes the study will prove to be beneficial in repairing hearing loss so other children can be treated successfully.
"As a mom of special needs, if you're able to help a child it's huge," she said. "There's nothing that can compare to giving a child back something that's been taken away."
Posted:
7/12/2012 4:16:20 PM by
Don Margolis | with
0 comments